What is Visual Acuity?
When you have an eye test, your visual acuity is one of the things that will be assessed, but what exactly is visual acuity? The term ‘Visual Acuity’ describes the smallest detail that a person can see when looking straight at a high contrast, stationary target. Visual acuity would be the most widely recognised measure of vision, though certainly not the only one, and not even necessarily the most important one (more on that in a future post). Visual acuity is usually reported in a standard format, and looks like a fraction where the nominator is usually ‘6’. The nominator tells you the distance the test was performed at, or is referenced to, while the denominator provides a comparison to the accepted ‘normal’ level.
The image shows a 6/12 fraction. There is an arrow connecting each number with a text box. The text box connected to the 6 nominator reads: this is the distance at which the person being tested was just able to distinguish the target. The text box connected to the 12 denominator reads: this is the distance from which a person with textbook normal vision would just be able to distinguish the target.
If your visual acuity is 6/12, it means that, standing at a distance of 6m, you can just decipher detail that someone with ‘normal’ vision could just decipher at a distance of 12m, i.e. you need to be twice as close (half the distance) in order to make out the detail, compared to the person with normal vision. 6/12 is classed as mild vision impairment.
6/6 is regarded as ‘normal’ vision. If you have 6/6 vision, it means that if you were to stand at 6m, you would be able to just pick out detail of a target that someone with ‘normal’ vision could also just distinguish at 6m. You may have come across the term ‘20/20 vision’, this is the American equivalent of 6/6, the same measurement expressed in feet, rather than meters.
Testing at different distances
We don’t always perform testing at a distance of 6m, in fact, it’s pretty unusual to do so, since most optometry practices don’t have rooms that are 6m long, but because this 6-notation is widely recognised, we usually convert the acuity fraction to this format. Many optometry practices use digital acuity charts, which can be calibrated so that the letters or symbols are labelled with the equivalent 6m value, even though you may be being tested at a shorter distance.
Children usually perform better at closer distances, so most of the more traditional board-type acuity charts are calibrated for use at 3m. We can report the acuity for the 3m distance, or convert to 6m, or both. It is best practice to report the distance at which the testing actually took place, this is because, while the same letter presented at 6m will be exactly half the size of a letter presented at 3m and therefore equivalent in theory, in practice, vision is more complex than that, and there are various reasons why someone who can read a particular target at the 3m distance may not be able to decipher the equivalent size letter when presented further away.
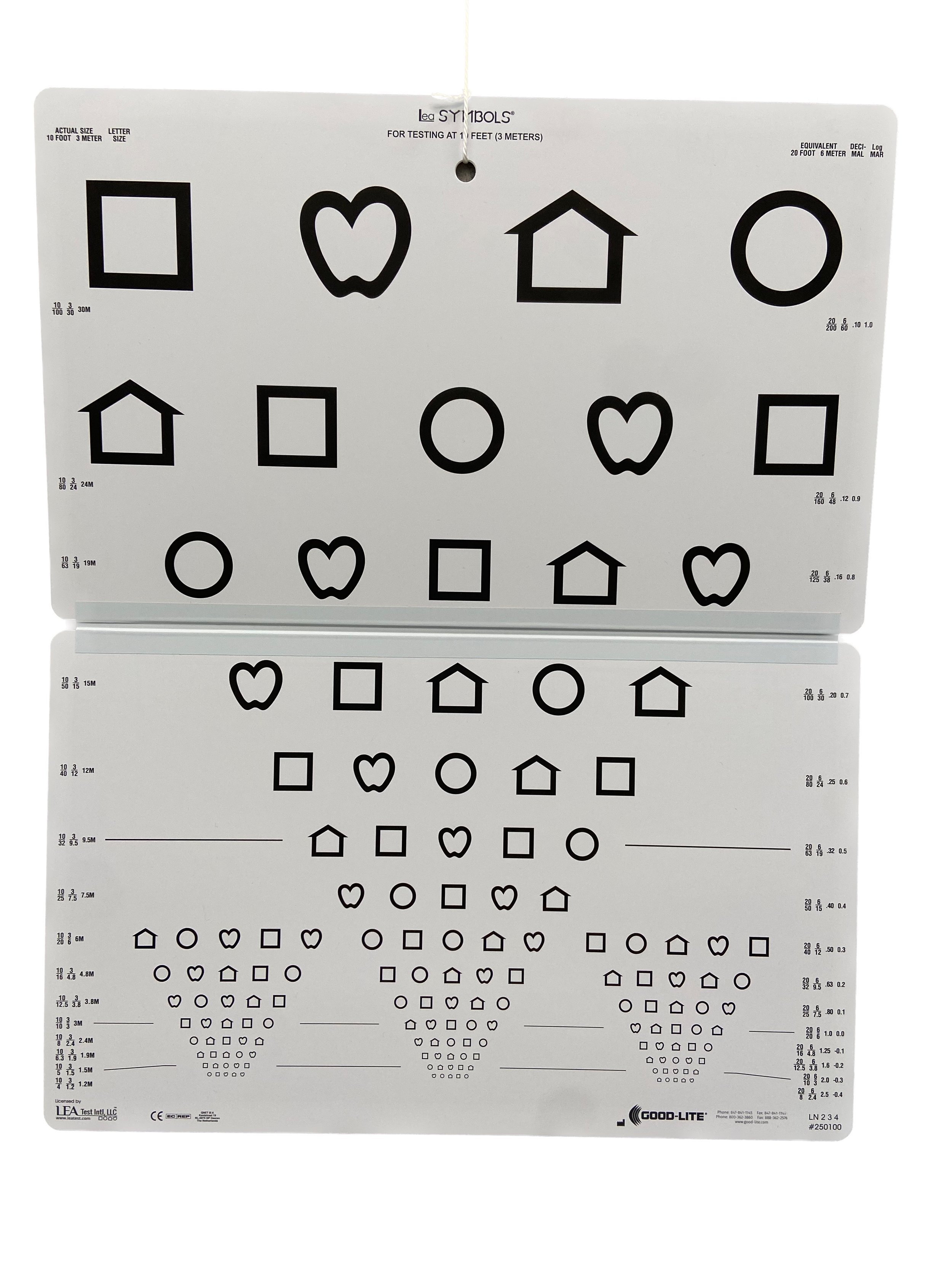
Image of a Lea Shapes 'board'-type visual acuity chart. The Lea chart is designed for use at 3m, since this distance is better for children
We might test a child at 3m, and measure their acuity as 3/9. in this situation, we could just report an acuity of 3/9, or we could report the equivalent 6 notation acuity which would be 6/18. The best way to record this finding would be to state that acuity was measured at 3m and recorded as 3/9, which is equivalent to 6/18.
Monocular or binocular
We can measure acuity monocularly, or binocularly. Monocular means with one eye, while binocular acuity is with both eyes. In clinical settings, we would typically measure acuity monocularly, since we want to measure the vision in each eye, to make sure it is not reduced in either eye. If vision is reduced in one eye, this may be because the eye is short or long-sighted, or it could be a sign of eye disease, such as a cataract, or changes at the back of the eye.
Image of a little girl, sitting in an optometrist's chair. She is wearing plastic glasses with a hinged occluder attached to each side. Her left eye is covered by the occluder and she is looking towards the camera with her uncovered right eye.
In low vision settings, we tend to be more interested in binocular visual acuity, because we want to understand the person’s habitual level of functioning, and for most of us, we are usually using two eyes in everyday life.
Other acuity measures
Acuity charts that contain letters or shapes measure ‘recognition’ acuity, i.e. can you recognise the shape or letter. If someone is unable to access the typical ‘recognition’ acuity charts, we move to ‘detection’ acuity charts. For these assessments, we are simply determining if the person can detect a visual target, such as black and white stripes. These tests are essentially easier to perform, and as such, their results are not directly comparable. If someone were to perform both tests, they would likely score higher on the detection (stripes) test, when compared to the recognition (letter) test.
Image of three of the visual targets from the Lea paddles acuity test. Each target is shaped like a ping-pong bat, with a handle for the examiner to hold, and a circular 'paddle' on top. The left target is plain grey, the middle target has narrow black and white stripes, and the right target has wide black and white stripes
For this reason, it is recommended that the detection tests be reported differently. They are graded by the number of ‘cycles’ per cm, where a cycle is defined as one black and one white stripe. From the perspective of understanding a person’s level of functioning, it is more useful to know that they can just decipher high contrast black and white stripes of width 0.25cm, from a distance of 1m, because we can extrapolate this information into everyday life situations. If they have black canvas shoes with white laces, they will probably be able to see their shoelaces when they bend down. If they have a knife and fork with a black handle, placed on a white tablecloth, they should be able to find their knife and fork when they sit down to a meal, because the handles will be wider than 0.25cm. If someone is using a communication system, such as a PODD or PECS system, this information is essential knowledge; without it, we cannot be sure that the person can actually see the images they are being expected to use to communicate their needs.
Close-up of a 2 cycles per cm Lea paddle with a ruler placed on top. There are two 'cycles' of black and white stripes across a width of 1cm.
Vision vs visual acuity
When measuring what a person can see, we usually measure both with and without their glasses or contact lenses. We use the term ‘vision’ to describe their uncorrected acuity i.e. what they can see when they are not wearing their glasses or contact lenses. Visual acuity is the vision level when their refractive error (short or long sightedness) is corrected by glasses or contact lenses. Best corrected visual acuity (BCVA) is measured after we have determined a person’s script i.e. when they have the optimum correction.
So during a routing eye exam, we might:
Ask you to remove your glasses and read the letter chart: measuring your vision
Get you to read the letter chart with your current glasses: measuring visual acuity
Measure your refractive error and then get you to read the chart again: measuring your best corrected visual acuity.
Visual acuity levels
As discussed above, 6/6 is considered ‘normal’, and any fraction where the denominator is smaller, e.g. 6/5, 6/4, 6/3, is considered good vision. Someone with 6/9 vision would also be considered within normal range.
If a person has acuity of worse than 6/12, i.e. the denominator is 12 or bigger, then they are considered to be visually impaired.
A person with acuity of 6/12 to 6/18 is considered to have a mild visual impairment
A person with acuities of worse than 6/18 to 6/60 is considered to have a moderate visual impairment
A person with acuities of worse than 6/60 is considered to have a severe visual impairment
But, there is more to vision….
It is important to remember that visual acuity measures one particular aspect of vision. Some people can have normal, or near normal visual acuity, but because other aspects of their vision are not working as we typically expect, they may experience significant challenges to seeing. in a future blog post I will talk more about other vision measures.
If you are interested in learning more about eye tests for someone with complex disability and/or addition needs, please get in touch via phone: 07 3544 6167, or email: reception@specialeyesvision.com.au.